Pneumonia: Lung Infection Disease
Pneumonia is a disease of the lower respiratory system, most often caused by bacteria, but also viruses. It can be dangerous, especially for young children, under the age of two and the elderly. In both cases, an urgent medical consultation for lung infection is most often required. Until the 20th century, pneumonia was the most common disease that led to death. The discovery by Louis Pasteur of the bacteria that cause pneumonia, followed by antibiotics by Alexander Fleming, resulted in a breakthrough in the treatment of the disease. What is pneumonia and how to treat it?
Table of Contents
What is pneumonia?
Pneumonia is inflammation of the lung parenchyma (air sacs of the lung or interstitial tissue) causing characteristic effusion. It results in a reduction in the area of the lungs, the appearance of shortness of breath in the chest, rapid breathing, or cyanosis, a symptom of which may be a bluish discoloration of the skin, nails, or mucous membranes.
Types of pneumonia
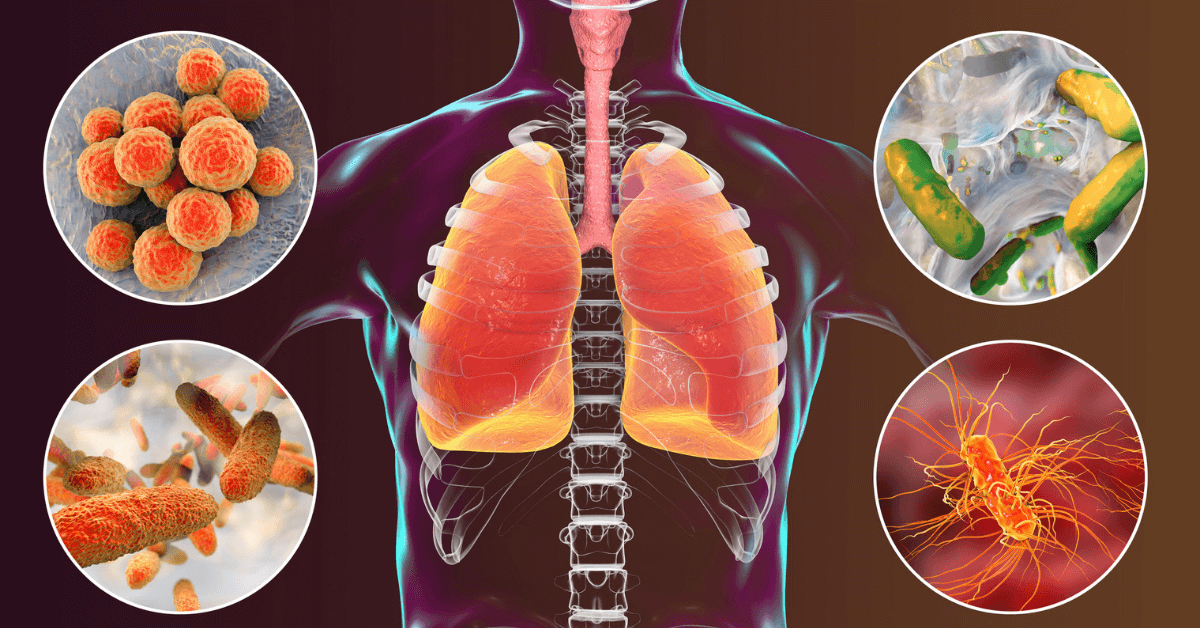
When classifying pneumonia according to the causative agent of the disease, the following types can be distinguished:
- bacterial, most common, occurring in more than 70% of cases, caused by Gram (+) and Gram (-) bacteria or anaerobic bacteria such as pneumonia; the most common bacteria causing pneumonia are S. pneumonia and H. influenzae,
- viral, constituting approx. 5-20% of cases of disease and caused by e.g. influenza virus, rubella, measles, adenovirus or coronavirus,
- parasitic, caused by Toxoplasma gondii, Strongyloides stercoralis, Plasmodium malariae, and Ascaris lumbricoides.
- fungal (candidiasis), caused by infection with Candida albicans or Aspergillus fumigatus,
- allergic, caused by environmental allergens,
- chemical, including greedy, so-called Mendelson’s syndrome caused by bacteria, common in gastroesophageal reflux
- idiopathic (idiopathic) pneumonia, a disease of the air sacs in the lungs that causes inflammation and then fibrosis causing increasing difficulty in breathing; its causes are still unknown to doctors.
There are also types of pneumonia, taking into account the location of inflammation:
- bronchial (lobular, lobular), usually starting with bronchitis and caused by the penetration of microorganisms into the lungs through the walls of the bronchi damaged by inflammation;
- lobar (croup), hematogenous inflammation that affects the entire lobe of the lung and the pleura covering it at the same time, caused by a bacterium – Streptococcus pneumonia,
- segmental, in which the inflammation extends to specific segments of the lung.
Another classification of pneumonia depends on the site of onset:
nosocomial pneumonia caused by infection with bacteria (Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumonia, as well as Staphylococcus aureus or Streptococcus pneumonia), which are found in hospitals and are resistant to most antibiotics used, which requires the use of stronger drugs;
The causes of pneumonia
Pneumonia is often preceded by bronchitis. This disease is particularly vulnerable to weakened people who have undergone surgeries whose organism is exhausted. Bronchopneumonia may be caused by prolonged hyperemia due to the weakening of the circulatory system. It can be especially dangerous for unconscious patients, whose respiratory tract and lungs have foreign bodies.
Other causes of pneumonia include inhalation of dust or other poisonous substances (chlorine, phosgene, mustard gas) and cigarette smoke, and the most common bacterial pneumonia is a bacterial infection.
Pneumonia and the coronavirus
Infection with COVID-19 coronavirus in many cases causes acute interstitial pneumonia, which can also lead to irreversible changes in the lungs. Inflammation in the lung parenchyma, especially in the space around the alveolus, causes its remodeling, combined with the destruction of the alveoli and their fibrosis. People with COVID-19 may experience severe flu-like symptoms, such as:
- muscle aches,
- sore throat,
- the general feeling of being unwell
- rapidly increasing shortness of breath.
In the acute course of COVID-19, patients may suffer from acute respiratory failure that requires treatment with a ventilator. Even after recovery, fibrosis and cavities in the lung tissue may be a trace of a history of the disease.
Factors predisposing to pneumonia
Your risk of getting pneumonia may be increased by factors such as:
- prematurity,
- old age,
- allergies or congenital defects of the respiratory system,
- chronic diseases, e.g. chronic obstructive pulmonary disease,
- diseases of the immune system or an immature immune system in children,
- airway obstruction,
- habitual smoking or excessive exposure to cigarette smoke,
- alcoholism,
- eating disorders,
- food content aspiration,
- disorders of the mucociliary system,
- the use of certain immunosuppressants
- The most common symptoms of pneumonia are:
- higher temperature,
- chills,
- sweating
- a feeling of general breakdown and weakness of the body,
- cough, during which purulent discharge of a yellow, gray, or green color is expelled,
- pain in the chest, generally in the lateral parts of the chest, worsening with deep breathing and coughing.
- With viral pneumonia, the above symptoms may also be accompanied by:
- sore throat,
- hoarseness,
- runny nose,
- muscle aches.
Symptoms of pneumonia that should urgently consult a doctor are:
- difficulty breathing and shortness of breath
- feeling sudden and severe pain in the chest,
- persistent fever above 39 ° C for more than three days,
- persistent cough during which the patient coughs up purulent discharge.
In young children, the symptoms of pneumonia are similar to those in adults. In addition, they may experience cyanosis – bluish skin on the fingers and around the mouth. In infants, pneumonia may be suspected when they become more weeping and their breathing becomes faster.
How to recognize pneumonia? Research and diagnostics
When making a diagnosis of pneumonia, the doctor, first of all, conducts a careful interview and performs a physical examination that allows you to hear the crackling and rattling of the lungs. The patient’s chest X-ray is also taken, showing the darkening of the lung parenchyma. An X-ray image is also performed as a follow-up examination after pneumonia has been cured. A more detailed examination for pneumonia is computed tomography of the chest, which allows you to obtain accurate images of any part of the body.
Additional diagnostics allowing for the diagnosis of pneumonia sometimes also includes blood tests: morphology and acute phase indicators – CRP, ESR, PCT. Bronchoscopy is performed in patients with severe or nosocomial pneumonia. During this procedure, the material from the respiratory tract and the pleural cavity is cultured and subjected to bacteriological examination. Its result makes it possible to identify the pathogens causing the disease, which enables the implementation of optimal and effective treatment.
Prevention of Pneumonia
Maintaining a healthy lifestyle and boosting your immunity naturally are the most effective actions in preventing pneumonia. If you want to protect yourself against this disease, it is worth remembering:
- a well-balanced diet rich in natural antibiotic foods such as garlic, spicy spices, millet, vegetables, and fruit;
- regular physical activity at least 5 times a week for 30 minutes;
- sleeping at least 7 hours a day;
- choosing clothes according to the weather and protecting hands and head from overcooling, and legs from getting wet;
- walks in the fresh air,
- avoiding stressful situations,
- the frequent airing of rooms,
- avoiding crowds.
Regular flu vaccinations and Streptococcus pneumonia vaccinations for people at risk (young children, the elderly, chronically and permanently immunocompromised people) are also effective practices to reduce the risk of developing pneumonia.
How is pneumonia treated?
When treating bacterial pneumonia, antibiotics are essential. During antibiotic therapy, one should not forget about the use of protective drugs and the consumption of large amounts of products rich in live bacteria, such as kefirs or yogurts. In addition, the treatment of pneumonia in the lungs is symptomatic, supporting the recovery process, during which:
- antipyretic drugs,
- antitussive drugs that stop the cough reflex in the first phase of dry, tiring cough and thin the mucus and facilitate its expectoration in the second phase of wet cough,
- oxygen therapy,
- plenty of fluids.
If the patient does not require hospitalization, he or she should stay at home during treatment and rest a lot infrequently ventilated rooms. However, it is worth not staying only in bed, which worsens the ventilation of the lungs. In the absence of fever, it is advisable to go on short walks, which will contribute to better ventilation. For the duration of treatment, it is recommended to stop smoking, and in order to prevent the disease – completely quit smoking.
Is pneumonia contagious?
Pneumonia caused by bacteria and viruses is contagious. Its infection is favored by decreased immunity, short-term – caused by e.g. a cold, or long-term – in patients suffering from diabetes, AIDS, neurological disorders, or during the treatment of neoplastic diseases.
How long does pneumonia last?
For typical antibiotic-treated pneumonia, the disease duration is generally 7 to 14 days. Treatment for bacterial or atypical pneumonia is more difficult and longer, which can take up to 14 to 21 days.
Diagnostics in the treatment of pneumonia can be performed in LUX MED facilities throughout the country, both privately and at the National Health Fund. The advantages include short waiting times for an X-ray or computed tomography of the chest, high quality of the examinations performed, thanks to which you do not have to repeat them, and the ability to collect the results online without leaving your home